Category: News
-
Read CAN Connection – March 2025
Read our most recent newsletter here: https://can-acn.org/can-connection-march-2025/ Content:
-
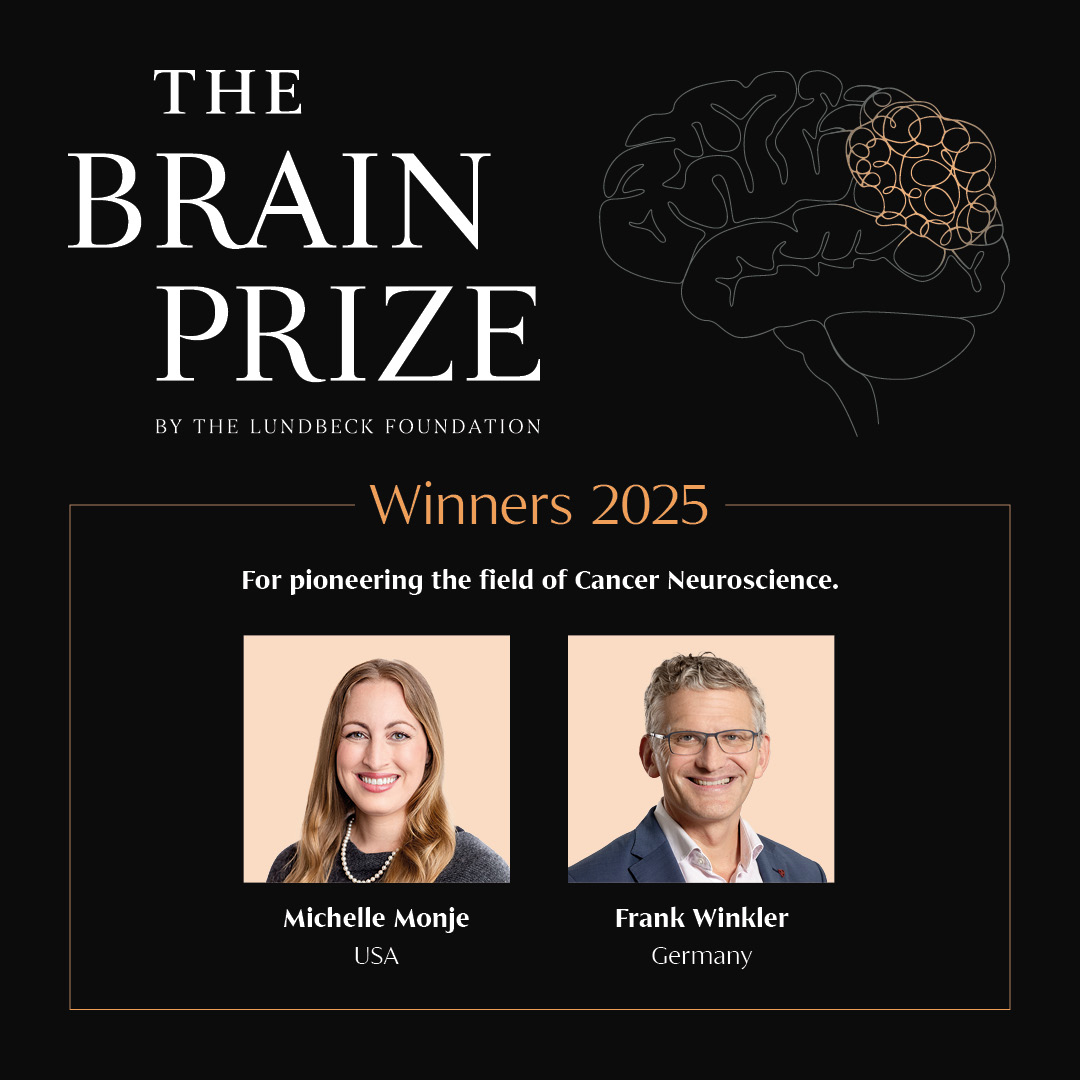
Congratulations to 2025 Brain Prize winners Michelle Monje and Frank Winkler
Pioneering research into brain cancer is awarded the world’s largest brain research prize, The Brain Prize Gliomas are types of cancers that arise in the brain and are extraordinarily difficult to treat. They are the leading cause of brain tumour-related deaths in both children and adults. Two pioneering scientists are awarded The Brain Prize 2025…
-
Read CAN Connection – December 2024 edition
Read the latest edition of our newsletter! CAN Connection – December 2024
-
CAN at the 2024 Canadian Science Policy Conference
The Canadian Association for Neuroscience was happy to participate in the Canadian Science Policy Conference last month in Ottawa, and in the symposium organized by the Canadian Brain Research Strategy: “Scaling Research for Impact: From Local Insights to Global Solutions“ on November 20, 2025. Read more about the symposium here: https://canadianbrain.ca/canadian-science-policy-conference-brain-health-and-research-summit-2024/
-
CAN submits a brief to the House of Commons Science and Research committee study on the Capstone Research Funding Organization Announced in Budget 2024
Read our submission to the House of Commons Science and Research Committee study on “The Mission, Mandate, Role, Structure and Financing of the New Capstone Research Funding Organization Announced in Budget 2024”
-
CAN Hill Day 2024
The Canadian Association for Neuroscience was proud to host its annual CAN Parliament Hill Day in Ottawa on November 5, 2024. It was a full day of meetings with elected officials and representatives of the main federal funding agencies to discuss how to better support scientific research in Canada.
-
The cellular secret of how memories are made, and lost
From: SickKids news Scientists use a peptide to strengthen connections between brain cells and restore memory in a pre-clinical model. Research led at The Hospital for Sick Children (SickKids) is illuminating the mechanism underlying memory, which could result in future therapeutic targets for conditions such as Alzheimer’s disease and dementia. Alzheimer’s disease is a condition…
-
Read our submission to pre-budget consultations
The House of Commons Standing Committee on Finance invited Canadians to participate in its annual pre-budget consultations process. The committee will table a report on these consultations in the House of Commons with recommendations to be considered by the Deputy Prime Minister and Minister of Finance in the development of the 2025 federal budget. Read…